OPINION: Racial bias has no place in medicine
Implementing diverse thinking in medical school curriculum can contribute to health equity
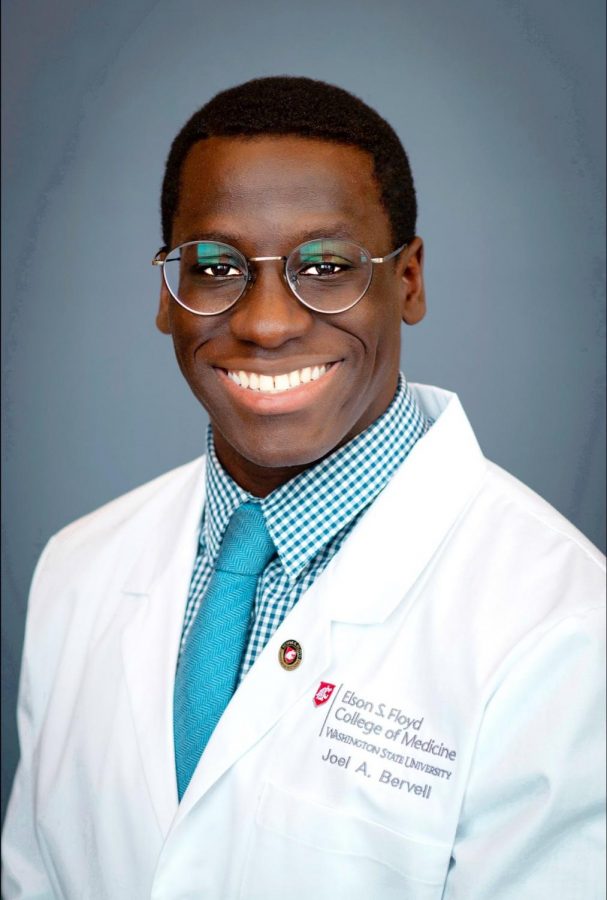
Joel Bervell, second year medical student and Medical Student Council President uses platforms on social media to spread awareness of racial bias in medicine.
March 11, 2021
A place that is synonymous with healing is not usually a forefront for scrutiny when thinking of racial inequality if you aren’t a person who has to deal with racism in the first place. Many times, racial biases are not perpetuated with the purpose of harming people, but instead are embedded in the education, technology and treatments used in clinical settings. Inadequate treatment, access to health care and poverty also go hand in hand with the pre-existing biases that altogether plummet the quality of life for people of color.
On top of this, the implicit biases that influence even medical judgment allow people to accept all information without further investigation. Overlooking information that is decades or centuries old allows the healthcare system to continually fail patients that fall under non-white categories.
As an example, Black patients are among the largest groups to suffer the consequences of racial bias in medicine. This has overall diminished the life expectancy of Black Americans to the lowest of any major group in the United States. As a developed country with all of these technological and industrial advances, this does not speak toward the mortality rates.
Many people unfortunately become familiar with these biases at a younger age. My father once told me about a time he felt some distrust in medical professionals. He didn’t feel like his concerns were important to the medical staff at the time.
My parents, teenagers at the time, had taken me to the emergency room when I was a few months old because I had a running fever they couldn’t manage. When we were admitted, an exam was conducted, and they asked for a urine sample. My parents were then left to wait for the doctor to come in with the results. After a long wait, the staff did nothing to alleviate my pain, and they were no longer checking in. My father went outside the room to try and get someone’s attention, but they seemed to be having a celebration in the staff room. After many attempts, my father gave up. My parents decided to take me home to try and care for me there.
An hour later, a sheriff showed up to our home and urged my father to take me back to the hospital because the doctor said I tested positive for a kidney infection. Afraid the doctors were going to continue to ignore us, my father told him why they decided to take me home, but the sheriff assured him that he would stay to make sure I was attended to. When we returned, the medical staff was waiting at the entrance, but that experience had already made a dent in my father’s trust.
This simple example exhibits how often people of color are overlooked in a medical setting. Whether it’s a language barrier, lack of medical literacy or a generalization that leads a medical professional to believe a patient of color is being overdramatic — it all leads to nothing but negative consequences for the patient.
Joel Bervell, second year medical student and president of the Medical Student Council at Elson S. Floyd College of Medicine, said he was aware racial bias was a serious issue in medicine throughout his general education.
“There were so many incidences where we talked about issues of race, and how medicine has disproportionately affected people of color,” Bervell said. “When I got to medical school, I continued to see them, maybe in more insidious ways.”
One of the many things Bervell became aware of was the fact African Americans spend much more time waiting to receive a kidney transplant than white patients. This is because of glomerular filtration rate, an outdated numerical system used in kidney medicine to calculate the number of working nephrons. Often, labs and doctors will adjust this number according to race, and African Americans happen to end up with higher values, putting them lower on the transplant list.
“I think one of the biggest things you’ll hear about often in medicine, is that many people don’t believe the pain of patients of color. And there’s been studies done on this,” Bervell said.
In one instance Bervell mentioned, Vanderbilt University conducted a study that involved asking medical students and residents false questions about beliefs they might have about Black individuals. The questions consisted of things, like “Do Black people have thicker skin?” or “Are the nerve endings of Black individuals different from the nerve endings of a white person?”
Shockingly, more than 50 percent of people answered at least one of those questions incorrectly, meaning they endorsed a false belief, Bervell said.
“Those people that endorse the false belief were more likely to also think that Black people didn’t feel as much pain,” Bervell said. “And that has real-world consequences.”
This often results in Black individuals and people from lower socioeconomic statuses being less likely to receive pain medications they need after a surgical procedure, Bervell said. This is because doctors may think they’ve dealt with patients like them before, they think the patient is overreacting or they don’t think the patient is telling the truth.
A generalization that can also keep patients from receiving proper care is characterizing drug-seeking behavior in people from low-income societies. Many times, they don’t have the language to be able to talk to the doctor about how they can receive the care they deserve, Bervell said.
“Much of medicine, and much of life, is just relating to people that are similar to you,” Bervell said. “So when you see someone from a different class of life, or someone that has been raised differently, you are not able to accurately associate with them, and empathize in the right way with those individuals.”
Another way medical bias is perpetuated in medicine begins during medical education. A recent study from the New England Journal of Medicine found that one of the things medical schools teach is how to use heuristics, or mental shortcuts to get to an idea, Bervell said.
One of the shortcuts taught is using race as a proxy to understand a patient’s diagnosis, he said.
“Many times, [medical] schools don’t teach why these things exist. So I think when you jump to conclusions, you can make misdiagnoses when you’re not looking at the entirety of your patient,” Bervell said. “Instead you’re looking at their skin color and their race.”
As we look toward the future of medicine, Bervell said he believes being aware these biases are perpetuated would help immensely because many people don’t know these things are out there.
“The next thing I’d say is it means bringing people to the table that are experiencing these things, so that we can record revenue on a community level and also on a national level,” Bervell said. “But I think making sure we center the voices of those most marginalized only does good. It only betters care for everyone; it doesn’t make care worse at all.”
Diversifying the workforce is one more thing that will greatly contribute to health equity among all walks of life. Currently, only four percent of physicians are Black compared to the approximate 14 percent of the U.S. population, Bervell said. We need to have a workforce in medicine that reflects the population in the United States.
“People from those communities understand the needs, the social terms of health in the area, the access to food, the access to social workers or mental health resources and what the community needs actually are,” Bervell said. “Their stories are going to be the ones that guide the path forward.”